Glaucoma is a painful, blinding disease that by definition is an increase in the pressure inside the eye. It is a bummer of a disease, probably the worst one we see. Why? Because no matter what approach is taken to attack this disease, our goal is usually to delay, not prevent, vision loss. This doesn’t paint a real rosy picture. But as long as this is understood, then together we can make educated decisions on how we want to manage the problem. Let’s talk a little about this entity and see if I can make it a little easier to process.
ANATOMY
The eye is divided into two divisions, the anterior (or front) segment and the posterior (or back) segment. The posterior segment is filled with a firmer, gelatinous substance called the vitreous. The anterior segment is filled with fluid called the aqueous humor. The aqueous is produced by the ciliary body, which is behind the iris, and migrates forward through the pupil and out through the drainage angle that is in the peripheral part of the eye in front of the iris. Light from outside passes through the clear cornea, aqueous, lens and vitreous to hit the retina which then organizes and send a signal up to the brain via the optic nerve.
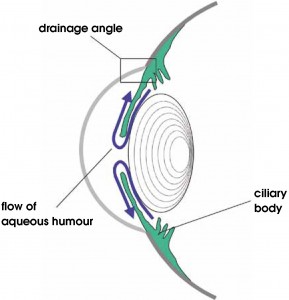
Pathway of aqueous humor
HOW DOES PRESSURE GO UP?
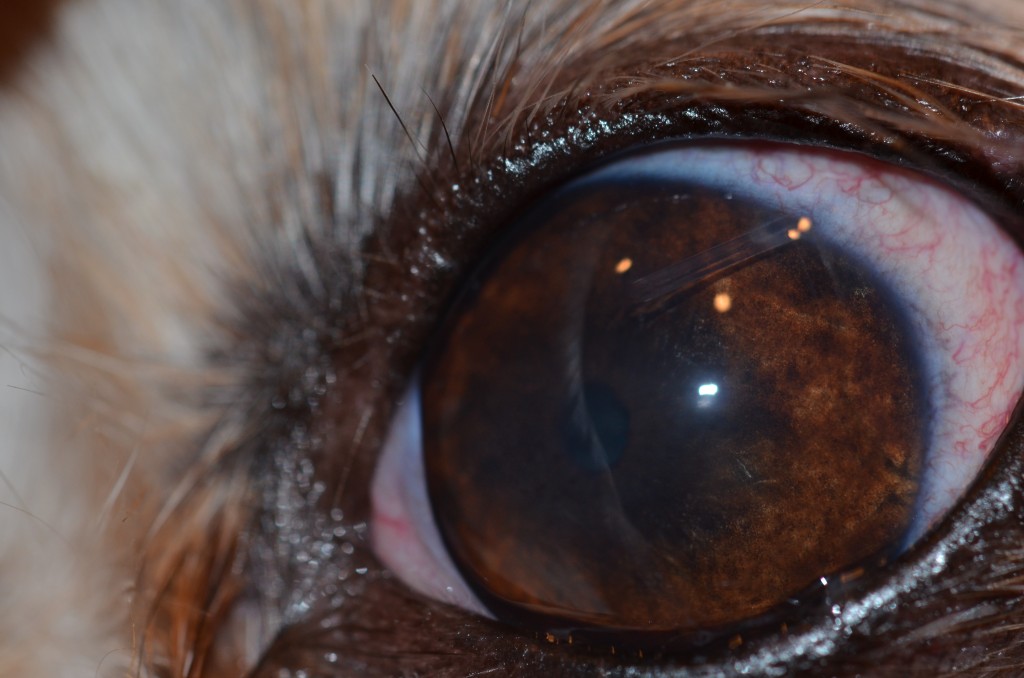
Trouble arises when this pathway of fluid from gland to drain becomes obstructed. Glaucoma comes in two flavors, primary or secondary. With primary glaucoma, the drain is abnormally formed and quits working sometime in adulthood without warning. In secondary glaucoma, the drain is normal but becomes obstructed with inflammatory debris, blood, lens material, tumor cells, etc., that will affect its function. The end result of both forms is the same which is an elevation of pressure inside of the eye since the gland continues to produce fluid that can’t escape outside the confines of the globe. The internal structures, and specifically the optic nerve, can’t handle pressure rise too well which results in damage. With the nerve, this results in peripheral vision loss initially that can progress to complete blindness. Steady elevation of pressure may go unnoticed in our pets as quality of vision is impossible to assess and they may not complain. However, if the pressure spikes rapidly, complete vision loss can occur in short order which is coupled with signs of pain, redness and haze.
You might think that we as owners will pick this up immediately and come rushing our pet into the hospital. Alas, this is not always the case. Dogs can fool us with vision loss in only one eye to the point where many are surprised when irreversible vision loss in the affected eye comes on the initial assessment. This speaks to two things. First is the disastrous nature of a high pressure rise and the minimal amount of time we have to truly recognize the issue, diagnose the problem and treat appropriately. Second is that we may perceive the redness and assume it is something simple like allergy or trauma that may go away on its own. We may take our pet into the hospital if improvement isn’t noted in a week or two which may be too late if pressure was up the entire time.
So what is the trigger? Well, many things depending on the cause. With primary glaucoma, the drain appears to quit working without warning or inciting cause in certain breeds. With secondary glaucoma, the list is long. Inflammation from trauma, immune-mediated disease, cataract formation, infectious diseases to name a few. We can see blood in the eye from trauma, clotting disorders, retinal detachment or tumors that obstruct the drain. Tumor cells themselves, or inflammation due to the presence of a tumor, can compromise the drain. The causes are varied and differ between species as well, with some entities more likely in one versus another. This creates a confusing and challenging dilemma for both owner and doctor to determine the underlying etiology.
To top it off, primary glaucoma is a disease of both eyes but is usually not symmetrical. Thus, we may lose with the first eye, especially if detected late in the course of the disease, and still have to concern ourselves with the time to onset in the remaining eye. This may not be the case with secondary glaucoma where the second eye may not necessarily be at risk if the cause of the pressure rise is unique to the affected eye. Sometimes a primary benign ocular tumor with secondary glaucoma may be a “good” diagnosis because the other eye is not at risk.

TREATMENT:
Medical and surgical management of glaucoma is dependent on whether it is primary or secondary and if there is vision potential or not. In dogs with acute primary glaucoma where vision retention or recovery is an option, drugs are used to try to decrease the production of fluid or increase the ability of the fluid to exit the eye. Multiple drugs, given topically, orally or intravenously, are usually warranted due to the time sensitive nature of this disease. In general, you want to throw the “kitchen sink” at these eyes, hope the pressure drops, and then reduce drugs if possible while you assess if vision returns and pressure remains within a normal range. We occasionally with tap the eye and manually remove some of the fluid to get a jump start on the IOP as sometimes it is more effective to do this and then try to keep the pressure low with drug rather than try to drive the IOP down with drug. If pressure is tenuously controlled or IOP will not drop with drug, surgical options to focally destroy the gland with laser energy and placement of a man-made valve to help with outflow can be considered. Again, the long term prognosis is guarded to poor so our goal is to try and delay vision loss for as long as we can. This is usually a more aggressive disease than seen with humans since we are dealing with higher pressures in eyes that get more inflamed. Many of the procedures used in humans don’t work in the dog due to species variation.
Gonioimplant (valve) into eye at the 2 o'clock position
If you have secondary glaucoma, treatment is directed towards addressing this entity, like significant intraocular inflammation, along with addressing the pressure. Thus, systemic antiinflammatories may carry a greater importance here.
Unfortunately, most dogs and cats that present with glaucoma may already be out of that small window where vision can be recovered. In these cases, our goal is comfort and cosmetics over vision. Medical management as above may be utilized to see if we can control the pressure, and maintain comfort, with a manageable amount of drug. If not, surgical options to achieve these goals by either removing the eye, placing an ocular or orbital prosthesis, or injection of drug into the eye to destroy the gland are our options. Although these can sound drastic, our pets do fantastically with them by relieving the migraine headache pain associated with this disease. This discomfort may not be externally evident if chronic, i.e. not squinting or rubbing, but positive changes in temperament and personality are usually an obvious sign that they feel better. An extensive discussion of these procedures are found in a prior post titled “Losing an Eye: Its not as bad as you think”.